Serum Ferritin Level as a Prognostic Marker of 30 days In Hospital Mortality of Coronavirus Disease 2019 (COVID 19) Pneumonia at World Citi Medical Center: A Retrospective, Observational Cohort, Single Center Study
Abstract
Introduction
The COVID-19 pandemic continues to affect a large swath of the global population. The Philippine records four hundred seventy-four thousand sixty-four (474, 064) confirmed COVID 19 cases since December 31 2020. The COVID 19 pandemic recently highlighted the role of systemic hyperferritenemia as a major cause of death. In this study, we were able to correlate the serum ferritin level and predict 30 day in hospital mortality in COVID 19 pneumonia.
Objective
The aim of the study is to investigate the correlation between serum ferritin level and disease mortality in COVID19 pneumonia with subset analysis on demographics and co-morbidities of patients with COVID 19 pneumonia.
Methodology
We reviewed the records of all laboratory confirmed COVID 19 patients from World Citi Medical Center from April 2020 up to April 2021.A statistically significant sample size of seventy nine (79) admitted patients were used in this study. A serum ferritin level was assayed using electrochemilumenescence immunoassay with a Roche COBAS analyzer.
Results
Result showed that high ferritin level is associated with in hospital mortality. With ferritin level of 1437.07ng/ml, poor clinical outcome and in hospital mortality was considered. We also observed that demographics and co morbidities of patients in this study were significant to predict in hospital mortality. Further sub-analysis of co morbidities such as Hypertensive cardiovascular disease, Type 2 Diabetes Mellitus, Chronic kidney disease, Liver disease, Chronic obstructive pulmonary disease and Cerebrovascular disease showed poor outcome which were directly related to ferritin levels with p value of <0.0001.
Conclusion
This study has demonstrated that elevated ferritin levels were shown to correlate with 30 day in hospital mortality as well as medical comorbidities such as Hypertensive Cardiovascular disease, Type 2 Diabetes Mellitus, and chronic kidney disease have shown significant evidence for in hospital mortality.
Author Contributions
Academic Editor: Raul Isea, Fundación Instituto de Estudios Avanzados - IDEA, Hoyo de la Puerta, Baruta.
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2021 Allen M. Quirit, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
The disease outbreak of coronavirus disease -2019 (COVID-19) continues to affect a large swath of the global population 1. The Philippine records four hundred seventy-four thousand sixty-four (474, 064) confirmed COVID 19 cases after the Department of health (DOH) reported one thousand five hundred fourty one (1,541) additional cases last December 31 2020. The COVID 19 has recently highlighted the role of systemic hyperinflammation as a major cause of death1. A virally induced cytokine storm syndrome associated with a massive and overwhelming systemic inflammation, burdens a subgroup of patients with severe COVID 19 which lead to pulmonary inflammation and extensive lung damage2. The association between high ferritin levels and a more aggressive subset of these diseases may suggest a possible pathogenic role of this molecule as proposed by the concept of hyperferritinemic syndrome3. A hyperinflammatory environment has been a hallmark of COVID 19 infection and is thought to be a key mediator of mortality4. In this study, we were able to correlate the serum ferritin level and disease mortality in COVID19 pneumonia and predict in hospital mortality based on demographics and co morbidities.
Objective
General Objective
The aim of the study is to investigate the correlation between serum ferritin level and disease mortality in COVID19 pneumonia.
Specific Objective
Specifically, the aim of this study is to correlate the serum ferritin levels to demographics and co-morbidities of patients with COVID 19 pneumonia, admitted at World Citi Medical Center from April 2020 up to April 2021 and predict 30 day in hospital mortality.
Significance of the Study
This study will evaluate the usefulness of ferritin level in prognosticating COVID 19 pneumonia and helps in the assessment of patients who need more aggressive approach to management.. It will also evaluate the correlation between ferritin level and disease mortality in COVID 19 pneumonia.
Methodology
We reviewed the records of all COVID 19 admitted patients from World Citi Medical Center, a Tertiary General Hospital with 150 bed capacity and ISO certifications for Quality Management System, Environmental Management System, and Health and Safety Management from April 2020 up to April 2021. A stastically significant sample size of seventy nine (79) patients in hospital admission was used in this study. A retrospective observational cohort study was conducted to patients presenting at the emergency department with COVID 19 confirmed pneumonia diagnosis. Serum ferritin levels was assayed using an electrochemilumenescence immunoassay with a Roche COBAS analyzer. Of all the COVID 19 positive patients, only hospitalized patients with a ferritin level available over admission were included in the analysis. Patients who had a ferritin level obtained within three days of admission were considered also as acceptable ferritin result. In patients with multiple ferritin levels obtained, the one closest to admission was used for the admission ferritin.
Study Definition
We classified the patients and defined them as COVID 19 confirmed case based on WHO definition and available confirmatory test in our institution. COVID 19 confirmed patients are patients with SARS CoV-2 infection documented by Nucleic acid amplification test (NAAT) specifically positive for Nasopharngeal swab (NPS) or Oropharyngeal swab (OPS) Reverse Transcriptase Polymerase Chain Reaction (RT PCR) test.
The chest radiographs were interpreted by a board certified radiologist and for the purposes of the study, pneumonia was defined as the presence of a radiographic infiltrate in the lung parenchyma, by Chest X ray or Chest CT scan. No exclusion criteria were documented.
The clinical outcome of the present study was to evaluate the use of ferritin level as indicator of in hospital mortality in patients with COVID-19 pneumonia.
Data Collection
In this study, all patients were initially assessed in the Emergency Department where a blood sample was drawn and Chest radiograph was performed. Information from each patient was collected from Medical Electronic Diagnostic Imaging System (MEDISYS) at hospital admission including demographic data, co morbidities, and epidemiologic characteristics. Ferritin values were reviewed by the authors who extracted the data and checked by simultaneously. If data were missing from the records or clarification was needed, we obtained data by direct communication with attending doctors and other healthcare provider. The patient’s data privacy and confidentiality was strictly observed by putting password enhanced files during and after data collection.
Patients and Method
Inclusion Criteria
Filipino adult patient aged 19 to 65 years of age, who were admitted at World Citi Medical Center with RT PCR SARS CoV -2 positive result, pneumonia by Chest X-ray or Chest CT scan, and ferritin level results.
Exclusion Criteria
Patients with positive NPS/OPS for SARS CoV2 but with no evidence of pneumonia either by Chest X-ray or Chest CT scan, inconclusive serum ferritin results (i.e values reported in >1000ng/ml or <1000ng/ml), and patients who were not able to complete their hospitalization (i.e. transferred to other hospital or discharged against medical advice) or exceeded 30 days of hospitalization were all excluded (See figure 1).
Figure 1.Summary of Data extraction, Inclusion and Exclusion criteria. 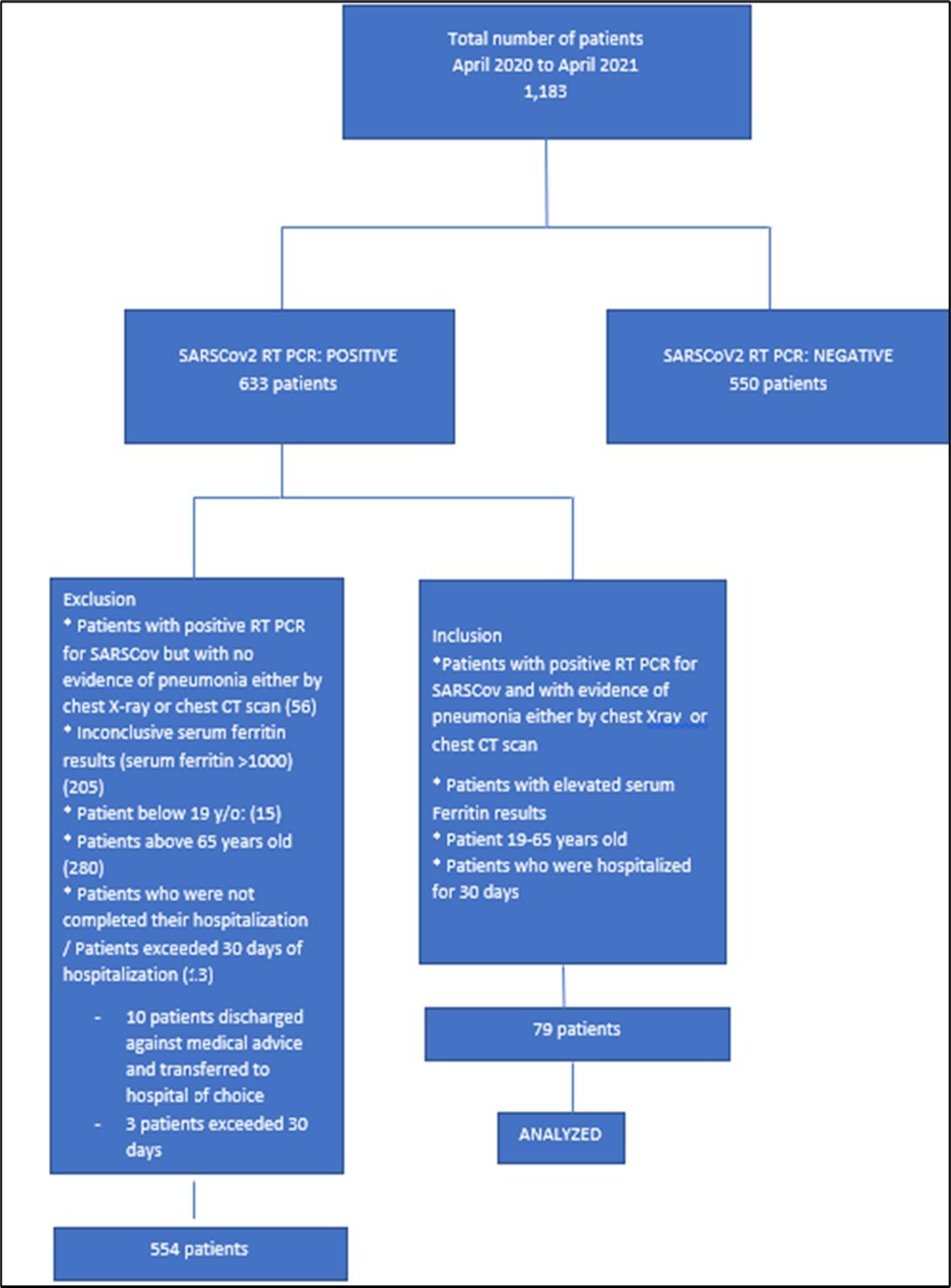
Sample Size
A minimum of seventy eight (78) patients were required for this study to predict thirty (30) days mortality among patients with COVID-19 pneumonia with 5% margin of error and 95% level of significance.
Data Extraction
We identified more than one thousand one hundred eighty three (1,183) patients by electronic search of which five hundred fifty (550) patients were excluded due to negative SARS CoV-2 RT PCR results. We retrieved the patient’s data for the remaining six hundred thirty-three (633) patients. Patients with positive RT PCR for SARS-CoV-2 but no evidence of pneumonia either by Chest Xray and Chest CT scan (56 patients); Inconclusive serum ferritin results (205 patients); patient below 19 years of age, and above 65 years of age (280 patients); patients who were not able to complete their hospitalization or exceeded 30 days of stay in hospital (13 patients) were all excluded. We retrieved the charts of the remaining patients who met all of inclusion criteria (79 patients) and were analyzed. (Figure 1)
Characteristics and demographics of the study population
A total of seventy nine (79) were included in this study. Patients aged 19 to 65 years (mean 45) were distributed evenly across different age groups. There was predominance of male gender (n= 46, 58.2%) than female (n= 33 (41.8%). Non-smokers (n=61, 77.2%) than smokers (n=18,22.78%) were observed. Their ferritin levels were discussed and correlated. (Table 1).
Table 1. Laboratory finding| Total | Non-survivors | Survivors | Univariable analysis | |||
| (n=79) | (n=14) | (n-65) | P value | OR (95% CI) | P value | |
| Ferritin | 709.16 | 1437.07 | 823.15 | <0.0001 | 0.219 (0.18 to 0.82) | <0.0001 |
Statistical Analysis
To summarize the demographic and clinical characteristics of the patients, descriptive statistic was used. Descriptive statistics were used to summarize the data in the form of frequency, percentage, mean and median ± interquartile range (IQR). Continuous variables were summarized as median (IQR) and categorical variables as absolute frequency. Summary statistics were performed for these data and grouping patients in survivors and non survivors in correlation to ferritin levels. A 5% significance level was used to test the results. Statistical analyses were performed using SPSS version 27 (SPSS) and R software. P values were calculated from the z value obtained. Differences between those groups were evaluated using Mann Whitney U test for quantitative variables and fischer’s exact test for categorical variables. (Table 2).
Table 2. Demographics (% and median value (IQR))| Total | Non-survivors | FLNS | Survivors | FLS | Univariable analysis | |||
| (n=79) | (n=14 or 17.7%) | (ng/ml) | (n-65 or 82.3%) | (ng/ml) | P value | OR (95% CI) | P value | |
| Demographics | ||||||||
| Age (years) | 45 (19-65) | 48 (19-65) | 1399.10 | 49 (24-64) | 1300.4 | 0.9473 | 0.14 (3.87 to 26.77) | 0.9823 |
| Male (%) | 58.20% | 71.40% | 1645.75 | 55.38% | 823.5 | <0.0001 | 1.29 (1.4 to 1.8) | <0.0001 |
| Female | 41.80% | 28.57% | 1069.75 | 44.62% | 823.15 | <0.0001 | 1.59 (2.2 to 3.5) | <0.0001 |
| Smokers | ||||||||
| Smoker | 22.78% | 21.43% | 1523.5 | 23.08% | 1489.6 | 0.9132 | 1.08 (4.33 to 4.67) | 0.916 |
| Non smoker | 77.22% | 78.57% | 823.5 | 76.92% | 820.5 | 0.9132 | 0.98 (1.27 to 1.3) | 0.9120 |
Results
Demographics and co morbidities for seventy nine (79) COVID 19 infections, who were admitted at World Citi Medical Center were included for analysis. Clinical characteristics are summarized in table 2 and ferritin results are presented in table 1.
Fourteen (17.7%) patients did not survive the thirty (30) days hospitalization. At the time of hospital admission, their baseline characteristics and differences were monitored in correlation with ferritin levels between patients who died and those who survived and discharged, including age 48 (19 - 65) vs 49 (24-64), with mean ferrin level for non survivor (FLNS) of 1399.10ng/ml vs among ferritin level of survivors (FLS) 1300.4 ng/ml respectively, OR 0.14; 95%( CI 3.87 to 26.77; p=0.9823), sex 71.40% vs 55.38% males, with mean FLNS of 1645.75ng/ml vs 823.5 FLS respectively, OR 1.29 95% (CI 1.4 to 1.8; p=0.0001), 28.57% vs 44.62 % females, with mean FLNS of 1069ng/ml vs 823.15ng/ml FLS respectively, OR 1.59 95% (2.2 to 3.5; p=<0.0001) and smokers 21.43% vs 23.08, with FLNS of 1523.5ng/ml vs 1489.6ng/ml FLS, OR 1.08 95% (CI 4.33 to 4.67 p=0.9132); non-smokers 78.57% vs 76.92%, with mean FLNS 823.5ng/ml vs 820.5 ng/ml FLS, OR 0.98 95% (CI 1.27 to 1.3 p=0.916) (table 2).
Specific comorbidities were also correlated to serum ferritin level. (Table 3), such as Hypertensive atherosclerotic cardiovascular disease (HASCVD) with mean ferritin level of 1187.78 ng/ml, five (5) patients out of eighteen (18) patients in this group did not survived with FLNS 1532.2ng/ml vs 623.5ng/ml FLS respectively with p value of <0.0001. Type 2 Diabetes mellitus with mean ferritin level of 1261.75 ng/ml, three (3) patients out of sixteen (16) patients did not survived with FLNS 1543ng/ml vs 1023.2 FLS with p value of <0.0001. Chronic Kidney Disease (with or without maintainance dialysis)with mean ferritin level of 1247.2 ng/ml, four (4) patients out of five (5) patients did not survived with FLNS of 1343.33ng/ml vs 1103ng/ml FLS respectively with p value of <0.0001. These top three co morbidities gave a significant impact to thirty (30) days in hospital mortality.
According to our results, consistent with previously published studies related to this paper, ferritin is associated with in hospital mortality as it is higher at the baseline admission of non-survivor patients and maintains significance after multivariable adjustment. With ferritin level of 1437.07ng/ml, poor clinical outcome and possible in hospital mortality was considered. (Table 1). We also observed that demographics and co morbidities of patients in this study were significant to predict thirty (30) days in hospital mortality. Further sub-analysis of co morbidities, HASCVD, Type 2 Diabetes Mellitus, Chronic kidney disease, Liver disease, Chronic Obstructive Pulmonary Disease and Cerebrovascular disease showed poor outcome which were directly related to ferritin levels with p value of <0.0001. (Table 3).
Table 3. Comorbidities (% and median value (IQR)| COMORBIDITIES | N | Fer.Level Mean | NS | FLNS | S | FLS | P value | Unvariable Analysis | |
| OR | P value | ||||||||
| Hypertensive atherosclerotic cardiovascular disease (HASCVD) | 18 | 1187.78 | 5(27%) | 1523.2 | 13(73%) | 623.5 | 0.0003 | 1.3 | <0.0001 |
| Chronic kidney Disease | 5 | 1247.2 | 4 (80%) | 1343.33 | 1 (20%) | 1103 | <0.0001 | 0.13 | <0.0001 |
| Diabetes mellitus | 16 | 1261.75 | 3 (19%) | 1543 | 13 (81%) | 1023.2 | 0.00023 | 2.2 | <0.0001 |
| Chronic Obstructive Pulmonary Disease (COPD) | 2 | 1264.5 | 1 (50%) | 1264.5 | 1 (50%) | 1264.5 | 1 | 0.5 | <0.0001 |
| Cerebrovascular Disease | 3 | 1370.67 | 2 (67%) | 1498.5 | 1 (33%) | 1115 | <0.0001 | 0.25 | <0.0001 |
| Liver pathology (cirrhosis) | 3 | 496.7 | 1 (33%) | 1000 | 2 (67%) | 583 | <0.0001 | 1 | <0.0001 |
| Human Immunodeficiency virus (HIV) | 1 | 1639 | 1 (100%) | 1639 | 0 | 0 | <0.0001 | NA | N/A |
| Pulmonary Tuberculosis (PTB) | 3 | 853.33 | 0 | 0 | 3 (100%) | 853.33 | <0.0001 | NA | N/A |
| Bronchial asthma | 2 | 496.5 | 0 | 0 | 2 (100%) | 496.5 | <0.0001 | NA | N/A |
| Dilated cardiomyopathy | 1 | 1460 | 1 (100%) | 1460 | 0 | 0 | <0.0001 | N/A | N/A |
| Hyperthyroidism | 1 | 110 | 0 | 0 | 1 (100%) | 110 | <0.0001 | NA | N/A |
| Cancer (breast) | 2 | 866.12 | 0 | 0 | 2 (100%) | 866.2 | <0.0001 | NA | N/A |
| Obstructive sleep apnea (OSA) | 1 | 978 | 0 | 0 | 1 (100%) | 978 | <0.0001 | NA | N/A |
| Acute coronary syndrome | 2 | 1675 | 2 (100%) | 1675 | 0 | 0 | <0.0001 | NA | N/A |
Discussion
At present, the pathophysiology, disease evolution, diagnosis and prognosis of patients with COVID 19 pneumonia are still unclear. In one study Dahan, et al,7 they concluded that elevated ferritin levels were shown to correlate with disease severity in 39 patients from Israel with confirmed COVID 19 infection. Severe patients had significantly higher level of ferritin (2817.6ng/ml) compared to non-severe patient (708.6ng/ml) p=0.02. In another released study of Moudhi et al,11 they concluded that elevated ferritin level >1000 were found to be an independent predictor of in hospital mortality. In one study of Zhoe et al,9 with 20 COVID -`19 patients, it was found that individuals with severe and very severe COVID-19 exhibited increase serum ferritin level, being serum ferritin the very severe COVID 19 group significantly higher than in the severe COVID -19 group (1006.16 ng/ml (IQR: 408.265-1988.25) vs 291.13ng/ml (IQR:102.1-648.42), respectively). In our study, we focused more on mortality outcomes to prognosticate patient during their admissions based on the ferritin levels. In this study, we were able to correlate the ferritin mean levels of survivors to non survivors (Table 1). At ferritin level of 1437.07 ng/ml, the prognosis of in hospital mortality may be predicted. Ferritin levels and prognostication of in hospital mortality may differ based on the co - morbidities at the time of admission (Table 3). Hypertensive Atherosclerosis Cardiovascular disease, Chronic kidney disease and Type 2 Diabetes Mellitus were the top three diseases that affect the mortality of the patient. Among other diseases listed in this table (Table 3), these three mentioned diseases got the higher levels of ferritin aside from acute coronary syndrome and cerebrovascular disease. In light of this data, we postulated that ferritin levels can be used as prognostic factor for in-hospital mortality. In plasma, ferritin circulates as apoferritin, a non-iron containing molecule. The plasma level generally reflects overall iron storage, with 1ng of ferritin per ml indicating approximately 10mg of total iron stores5. Due to its crucial role in cellular iron hemostasis, it is not surprising that ferritin synthesis is tightly regulated6. It has been well established that elevated serum ferritin levels may suggest not only the presence of an iron overload state but is also a marker for inflammatory, autoimmune, infectious or malignant conditions.7. The pathogenicity of the novel SARSCoV-2 and its effects on the immune system has yet not been completely understood. However, some studies with evidence suggest that severe progressive COVID-19 disease is associated with uncontrolled inflammation and massive cytokine release 7. It is also associated with immunological abnormalities, including cytokine storm and hyperferritinemia. 8. In agreement with this, another study revealed that in patients who died by COVID -19, ferritin levels were high upon hospital admission and throughout the hospital stay10. From these collected data, we postulated that ferritin level on the day of admission, can be used as prognostic marker of hospital mortality of COVID 19 pneumonia. .12
Conclusion
This study has demonstrated that elevated ferritin levels were shown to correlate with 30 day in hospital mortality among seventy-nine (79) patients admitted at World Citi Medical Center. Ferritin is readily available, measurable, cost effective and reliable test that could be very useful in establishing the risk of hospital mortality and guiding therapeutic decision in patient with COVID 19 infection. Patients who have medical comorbidities such as Hypertensive Cardiovascular disease, Type 2 Diabetes Mellitus, and chronic kidney disease have shown significant evidence for possible in hospital mortality. .13, 14, 15
Recommendation
More studies with higher populations will be needed to support the use of ferritin levels as marker for 30 days in hospital mortality for COVID 19 pneumonia. A larger multicenter cohort study from various hospitals of the country would help to further validate the findings of our study, however, with the evidence we have, serum ferritin levels could be implemented in the prognostic evaluation of in hospital mortality for COVID 19 pneumonia. Further studies are needed to evaluate if high values of serum ferritin in patient with COVID 19 pneumonia could be related to other comorbidities and optimum timing of ferritin analysis could improve outcomes. It would be useful to have an exact value of serum ferritin levels in our institution rather than repeated values of >1000 would be helpful. .16, 17
Limitations
The study is limited by data from single center with moderate to critically ill COVID 19 pneumonia which may introduce a selection bias and inflate the mortality. Hence result from this study may help in the risk stratification and management of similar moderate to critically ill pneumonia only. COVID-19 pneumonia is a complex and not yet well established disease and it should be mentioned that other factors could influence final outcome. 18, 19
References
- 1.Merad Miriam, Martin Jérôme. (2020) Pathological inflammation in patients with COVID-19: a key role for monocytes and macrophages. , Nature Reviews Immunology 20, 1-8.
- 2.Ruscitti Piero, Giacomelli Roberto. (2020) Ferritin and Severe COVID-19, from Clinical Observations to Pathogenic Implications and Therapeutic Perspectives. The Israel Medical Association journal :. , IMAJ 22, 516-518.
- 3.Perricone Carlo, Bartoloni Elena, Bursi Roberto, Cafaro Giacomo, Guidelli Giacomo et al. (2020) COVID-19 as part of the hyperferritinemic syndromes: is there a role for iron depletion therapy?.
- 4.Feld Jonathan, Tremblay Douglas, Thibaud Santiago, Kessler Alaina, Naymagon Leonard. (2020) Ferritin levels in patients with COVID‐19: A poor predictor of mortality and hemophagocytic lymphohistiocytosis. , International Journal of Laboratory Hematology 42.
- 5.Escobar López, Alejandro, Madurga Rodrigo, Castellano José, Velázquez Sara et al. (2021) Risk Score for Predicting In-Hospital Mortality in COVID-19. , (RIM Score). Diagnostics 11.
- 6.Ciceri Fabio, Beretta Luigi, Scandroglio Mara, Colombo Sergio, Landoni Giovanni et al. (2020) Microvascular COVID-19 lung vessels obstructive thromboinflammatory syndrome (MicroCLOTS): an atypical acute respiratory distress syndrome working hypothesis. Critical care and resuscitation : journal of the Australasian Academy of Critical Care. , Medicine 22.
- 7.Dahan Shani, Segal Gadi, Katz Itai, Hellou Tamar, Tietel Michal et al. (2020) Ferritin as a Marker of Severity in COVID-19 Patients: A Fatal Correlation. The Israel Medical Association journal :. , IMAJ 22, 494-500.
- 8.Ramos-Casals Manuel, Brito-Zerón Pilar, López-Guillermo Armando, Khamashta Munther, Bosch Xavier. (2013) Adult haemophagocytic syndrome. , Lancet 383.
- 9.Zhou Peng, Yang Xinglou, Wang Xian-Guang, Hu Ben, Zhang Lei et al. (2020) A pneumonia outbreak associated with a new coronavirus of probable bat origin. , Jing & Luo, Yun & Guo, Hua & Jiang, Ren-Di & Liu, Mei-Qin & Chen, Ying & Shen, Xu-Rui 579.
- 10.Sarfaraz Samreen, Shaikh Quratulain, Saleem Syed, Rahim Anum, Herekar Fivzia et al. (2021) Determinants of in-hospital mortality in COVID-19; a prospective cohort study from Pakistan. , PLOS ONE 16, 0251754.
- 11.Meloni Marco, Izzo Valentina, Giurato Laura, Brocco Enrico, Ferrannini Michele et al. (2019) . Procalcitonin Is a Prognostic Marker of Hospital Outcomes in Patients with Critical Limb Ischemia and Diabetic Foot Infection. Journal of Diabetes Research 1-5.
- 12.V H Gutiérrez. (2016) Red cell distribution width: A marker of in-hospital mortality in ST-segment elevation myocardial infarction patients?. Revista Médica del Hospital General de. , México 80.
- 13.Escobar López, Alejandro, Madurga Rodrigo, Castellano José, Aguiar Santiago et al. (2021) Hemogram as marker of in-hospital mortality in COVID-19. , Journal of Investigative Medicine 69.
- 14.Sun Ying, Dong Yanli, Wang Lifeng, Xie Huan, Li Baosen et al. (2020) Characteristics and prognostic factors of disease severity in patients with COVID-19: The Beijing experience. , Journal of Autoimmunity 112.
- 15.Vargas-Vargas Manuel, Cortés-Rojo Christian. (2020) . Ferritin levels and COVID-19. Revista Panamericana de Salud Pública 44, 1-2.
- 16.Gómez-Pastora Jenifer, Weigand Mitchell, Kim James, Wu Xian, Strayer Jacob et al. (2020) product of inflammation or a pathogenic mediator?. Clinica Chimica Acta. Hyperferritinemia in critically ill COVID-19 patients – Is ferritin the 509.
- 17.Kim Jeong-Hoon, Kim Dae, Jeong In-Beom, Son Ji-Woong, Na Mun-Jun et al. (2018) Serum ferritin as a prognostic marker of pneumonia: a prospective, single center study. 2608.
- 18.Lin Zhi, long Fei, Yang Yong, Chen Xiangyu, Xu Linyong et al. (2020) Serum ferritin as an independent risk factor for severity in COVID-19 patients. , Journal of Infection 81.
- 19.Alroomi Moudhi, Rajan Rajesh, Omar Abdulaziz, Alsaber Ahmed, Pan Jiazhu et al. (2021) Ferritin level: A predictor of severity and mortality in hospitalized COVID‐19 patients. Immunity, Inflammation and Disease. , Hassan, Kobalava & Aboelhassan, Wael & Almutairi, Farah & Alotaibi, Naser & Saleh, Mohammad & AlNasrallah, Noor & Al‐Bader, Bader & Malhas, Haya & Ramadhan, Maryam & Abdullah, Mohammed & Abdelnaby