Abstract
Introduction
Globally, 36.7 million individuals live with HIV/AIDS, with 2.5 million new cases annually. Youth (14-25 years) account for 45% of these new infections. Those aged 15-24 years are less likely to be aware of their HIV status and engage in HIV care compared to older adults. This study explores the use of HIV self-testing to improve access to HIV care among Kenyatta University undergraduates.
Objective
To identify barriers and facilitators to HIV self-testing in this group.
Methodology
Employing multistage cluster sampling, 398 students were surveyed using a self-administered questionnaire.
Results
Of the participants (median age 21 years, 1:1.03 male-to-female ratio), 91.7% understood HIV's seriousness, with sexual intercourse as the primary transmission mode. Self-testing usage was 28.8%. Key barriers included fear of partner reaction, stigma, and lack of confidence. Significant facilitators were being female, knowledgeable about HIV, and sexually active.
Conclusion
Only 24% had prior HIV testing experience. The study highlights the importance of addressing fears and misconceptions while leveraging knowledge and sexual activity awareness to promote HIV self-testing.
Author Contributions
Academic Editor: Kapriolzzf, Flapper mod, Sweden
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2024 Nicholas Muendo, et al
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Globally, 36.7 million people live with HIV/AIDS, and annually, 2.5 million new infections are reported. Notably, 45% of these infections are among youth aged 14 to 25, with university students at high risk due to behaviour’s like cross-generational sexual relationships, escalating the spread of HIV/AIDS and other sexually transmitted diseases1, 2. HIV self-testing (HIVST) offers a private means for individuals, particularly university students, to test for HIV, thus enhancing testing access for high-risk groups 3. This method detects HIV-1 p24 antigen or HIV-1/2 antibodies, requiring healthcare confirmation for positive results and has a specificity of 99.9% 4. In Kenya, HIV/AIDS prevalence is noteworthy, with a 3.7% rate among adults aged 15 to 49, emphasizing the virus's significant impact, especially on the young population. This highlights the need for continued research and interventions 5. Despite the importance, HIV testing and linkage to care among adolescents and young adults are low, hindering epidemic control3. Insufficient awareness of HIV status and late treatment initiation among youth are leading to more infections6. HIVST could bridge testing gaps and foster preventive practices 7. This study investigates the obstacles to HIV testing among a demographic highly susceptible to the disease.
Materials and Methods
The study, a cross-sectional descriptive analysis, was conducted at Kenyatta University's main campus in Nairobi, Kenya. This campus was selected for its diverse student population.
A multi-stage cluster sampling method was used, selecting random clusters within faculties or schools. This approach was chosen to effectively represent the university's large and dispersed undergraduate population. The sample size, determined using Fischer's formula, was set at 398, accounting for a 95% confidence level, a 55% target characteristic proportion, and a 5% precision degree.
Participants included undergraduates aged 18-25 years at the main campus, excluding those who were HIV positive and on treatment or taking end-of-semester/year exams. Data collection involved self-administered questionnaires with both open and closed questions, piloted at the Parklands campus.Data analysis was quantitative, focusing on descriptive analysis and quantitative methods to explore variable relationships 8, 9. Ethical approval was obtained from the Kenyatta University ethics committee, and participant confidentiality was ensured.
Results
The average age of the participants was 21.1 years, with a majority being single, female, Christian, full-time students majoring in Education, and living off-campus (Table 1).
Table 1. Socio-Demographic Characteristics of the Study Participants| Socio-Demographic Characteristics | Frequency , n=398 | Percent% |
| Age (Years) | ||
| 18 – 21 | 257 | 64.6 |
| 22 – 25 | 141 | 35.4 |
| Gender | ||
| Male | 196 | 49.2 |
| Female | 202 | 50.8 |
| Marital status | ||
| Single | 390 | 98.0 |
| Married | 8 | 2.0 |
| Religion | ||
| Christian | 373 | 93.7 |
| Muslim | 25 | 6.3 |
| Mode of study | ||
|---|---|---|
| Full time | 391 | 98.2 |
| Part time | 7 | 1.8 |
| Residency status | ||
| In school | 137 | 34.4 |
| Out of school | 261 | 65.6 |
| School | ||
| Environmental Sciences | 7 | 1.8 |
| Business | 71 | 17.8 |
| Hospitality and Tourism | 17 | 4.3 |
| Nursing Sciences | 6 | 1.5 |
| Education | 122 | 30.7 |
| Engineering and Technology | 6 | 1.5 |
| Economics | 29 | 7.3 |
| Agriculture & Enterprise Development | 6 | 1.5 |
| Public Health and Applied Human Sciences | 24 | 6.0 |
| Pure and Applied Sciences | 32 | 8.0 |
| Medicine | 7 | 1.8 |
| Humanities and Social Sciences | 40 | 10.1 |
| Architecture | 6 | 1.5 |
| Creative, Film and Media Studies | 17 | 4.3 |
| Law | 8 | 2.0 |
Barriers to the use of HIV self-testing
Participants demonstrated substantial knowledge about HIV, recognizing it as a serious disease primarily transmitted through sexual contact. Nearly half were informed about HIV pre-exposure prophylaxis, the lack of a definitive cure, and the possibility of living a normal life with Highly Active Antiretroviral Therapy (HAART), as detailed in (Table 2). Participants had a favorable view of HIV self-testing; most had been tested within the past three months, including through self-test kits. While facility-based testing (VCT) was prevalent, a significant portion preferred the OraQuick self-test kit (Table 3). Among the 97 participants who used HIV self-testing, routine use and protecting loved ones were primary motivations. The predominant reason for avoiding testing was the fear of a positive result (Figure 1), while fear of stigmatization was the main obstacle to facility-based testing (Figure 2).
Table 2. Knowledge about HIV (HIV as a Serious Disease)| HIV/AIDS is a serious disease | Frequency , n=398 | Percent % |
| Yes | 364 | 91.5 |
| No | 18 | 4.5 |
| Unsure | 16 | 4.0 |
| How HIV is spread | ||
| Sexually | 390 | 98.0 |
| Mother to Child | 349 | 87.7 |
| Blood Transfusion | 327 | 82.2 |
| Intravenous Drug Abuse | 180 | 45.2 |
| Aware of Pre-exposure prophylaxis | ||
|---|---|---|
| Yes | 190 | 47.7 |
| No | 160 | 40.2 |
| Unsure | 48 | 12.1 |
| HIV has a cure | ||
| Yes | 20 | 5.0 |
| No | 341 | 85.7 |
| Unsure | 37 | 9.3 |
| Live normal life with HAART | ||
| Yes | 316 | 79.4 |
| No | 28 | 7.0 |
| Unsure | 54 | 13.6 |
| Ever tested for HIV | Frequency , n=398 | Percent% |
| Yes | 260 | 65.3 |
| No | 138 | 34.7 |
| Ever used HIV self-test kit | ||
| Yes | 97 | 24.4 |
| No | 301 | 75.6 |
| Last time tested for HIV | Frequency , n=260 | Percent% |
| Last 3 months | 69 | 26.5 |
| Last 6 months | 75 | 28.8 |
| More than 1 year ago | 116 | 44.6 |
| Type of test done at that time | ||
| Facility test (VCT) | 185 | 71.2 |
| HIV self-testing | 75 | 28.8 |
| HIV self-test used | Frequency, n=97 | Percent % |
| INSTI | 25 | 25.8 |
| OraQuick | 59 | 60.8 |
| Atomo HIV self-test | 13 | 13.4 |
Figure 1.HIV Testing Acceptance (Reason not to perform HIV test)
Figure 2.HIV Testing Acceptance (Facility Based HIV Testing Challenge)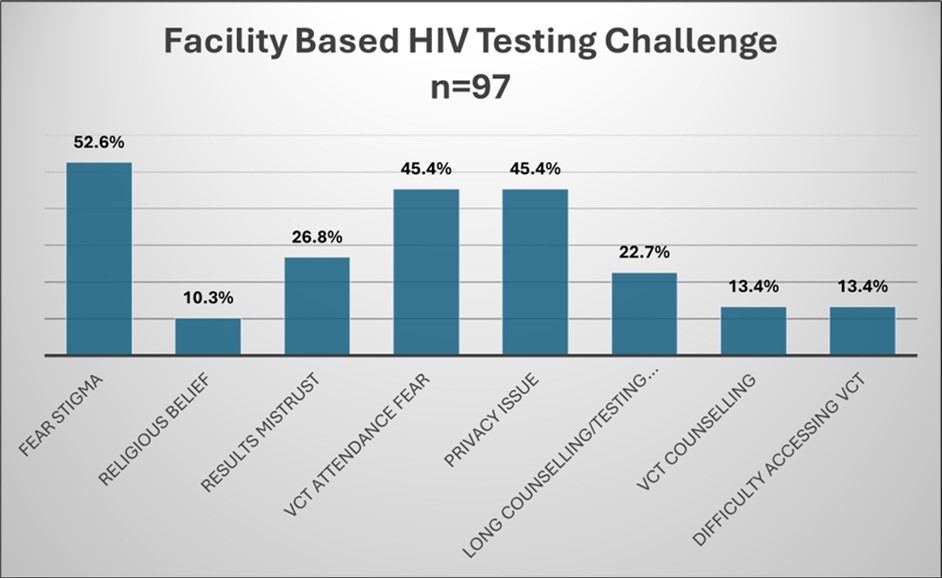
Facilitators to the use of HIV self-testing
Participants recognizing HIV/AIDS as serious and informed about pre-exposure prophylaxis, as well as those identifying as sexually active, were more inclined to use HIV self-testing (Table 4).
Table 4. Sexual behaviour factors| Ever had sex | Frequency , n=398 | Percent% |
| Yes | 278 | 69.8 |
| No | 120 | 30.2 |
| Consider self sexually active Consider self sexually active | ||
| Yes | 228 | 57.3 |
| No | 50 | 12.6 |
| Never had sex | 120 | 30.2 |
Media exposure, notably the "Chukua Selfie" campaign, correlated with higher usage of HIV self-testing. Participants generally favored self-testing and would recommend it to others (Table 5).
Table 5. Recommendation of HIVST and knowledge about “Chukua Selfie” HIVST Campaign| Knowaboutcampaigndubbed“ChukuaSelfie” | Frequency , n=398 | Percent % |
| Yes | 189 | 47.5 |
| No | 209 | 52.5 |
| Recommend HIV self-testing | Frequency , n=97 | |
| Yes | 97 | 100.0 |
Comparing barriers with facilitators in the uptake of HIV self-testing
Comparing barriers and facilitators for HIV self-testing among undergraduates, most participants hadn't used it, and no significant statistical link was found between demographic factors (age, gender, marital status) and self-testing usage (Table 6). However, several facilitators, such as knowledge about HIV/AIDS, awareness of pre- exposure prophylaxis, and considering oneself sexually active, were identified (Table 7)
Table 6. Barriers to the use of the HIV self-testing| Barriers to the use of the HIV self-testing | Everused,n=97 | Neverused,n=301 | OR (95% CI) | p-value |
| Age (Years) | ||||
| 18 – 21 | 60 (61.9) | 197 (65.4) | Reference | |
| 22 – 25 | 37 (38.1) | 104 (34.6) | 1.2 (0.7 – 1.9) | 0.520 |
| Gender | ||||
| Male | 40 (41.2) | 156 (51.8) | Reference | |
| Female | 57 (58.8) | 145 (48.2) | 1.5 (1.0 – 2.4) | 0.071 |
| Marital status | ||||
| Single | 94 (96.9) | 296 (98.3) | Reference | |
| Married | 3 (3.1) | 5 (1.7) | 1.9 (0.4 – 8.1) | 0.390 |
| Ever used, n=97 | Never used, n=301 | OR (95% CI) | p-value | |
| KnowledgeaboutHIV | ||||
| HIV/AIDS is a serious disease | ||||
| Yes | 93 (95.9) | 271 (90.0) | 1.2 (0.4 – 3.7) | 0.752 |
| No | 4 (4.1) | 14 (4.7) | Reference | |
| Unsure | 0 (0.0) | 16 (5.3) | - | |
| Aware of HIV Pre- exposure prophylaxis | ||||
| Yes | 64 (66.0) | 126 (41.9) | 3.4 (1.9 – 5.8) | <0.001 |
| No | 21 (21.6) | 139 (46.2) | Reference | |
| Unsure | 12 (12.4) | 36 (12.0) | 2.2 (1.0 – 4.9) | 0.052 |
| HIVhasa cure | ||||
| Yes | 3 (3.1) | 17 (5.6) | 0.5 (0.1 – 1.7) | 0.288 |
| No | 88 (90.7) | 253 (84.1) | Reference | |
| Unsure | 6 (6.2) | 31 (10.3) | 0.6 (0.2 – 1.4) | 0.205 |
Discussion
The study, mainly involving undergraduate students aged 18-21, may best represent this demographic. With almost equal gender representation, findings could apply to both males and females, echoing Hatzold et al.'s discovery of first-time testers among 16-24-year-olds 10. The high number of single, predominantly Christian participants indicates a focus on sexual activity and underlines the need for tailored HIV testing and prevention interventions, as also noted in studies by Buldeo et al. and others 11. The participants' status as full-time students suggests school-based interventions might effectively promote HIV testing and prevention, supported by evidence from relevant meta-analysis and systematic reviews 12. The dependence on family financial support, versus government or employment funding, underscores the importance of family in HIV prevention and aligns with findings from 13Basset et al., stressing the need to address financial barriers in healthcare access.
Barriers to the use of HIV self-testing
The study revealed satisfactory HIV/AIDS knowledge among participants, contrasting a Malaysian study showing limited understanding of non-HIV STDs and alarming risky behaviors 14. This aligns with a Sudanese study where sexually active students showed willingness to engage in safe sex practices 15. A significant number had undergone HIV testing, reflecting a positive testing attitude, similar to S. Marks et al.'s findings on HIV self-testing preferences among young men16. Major barriers identified were fear of positive results and access to self-test kits, paralleling Y. Qin et al.'s study, which found HIVST reduced stigma 17. Risky sexual behavior among some participants highlighted the need for enhanced safe sex promotion. Stigma was a barrier, resonating with Clifton et al.'s study on HIV risk perception and testing behavior in the British population, revealing a disconnect between perceived risk and testing behavior18 .
Facilitators to the use of HIV self-testing
The study found participants generally had positive attitudes towards those living with HIV, though some harbored fears and misconceptions. Media, especially social media, effectively raised HIV self-testing (HIVST) awareness, echoing Birdthistle et al.'s findings on the impact of a multimedia campaign in South Africa19. Participants valued the privacy and ease of interpreting self-test results at home. Accessibility and affordability of self-test kits were key, aligning with Y. Qin et al.'s research on reducing stigma through HIVST14. Repeat usage willingness was high among past self-test users, similar to the "4 Youth by Youth" Nigerian study by Iwelunmor et al. emphasizing youth engagement in HIV prevention20. Facilitators like HIV prevention education, routine testing, and protecting loved ones were also noted, supported by a study among African-American youths in North Carolina, highlighting these factors as enablers for self-testing 21.
Barriers compared with facilitators in the uptake of HIV self-testing services
The study showed 24% of participants had used HIV self-test kits, a moderate uptake akin to findings in Malawi and Zimbabwe among young people22. Female students' usage of self-testing was higher but not statistically significant, contrasting with Kenya AIDS Indicator Survey's higher reported testing in adolescent girls and young women23. Sexually active individuals were more inclined to use self-test kits, paralleling Izizag. B et al.'s findings on high acceptability among university students24. A tendency emerged where those with negative attitudes towards HIV-positive people were less likely to self-test, diverging from Kumwenda et al.'s study, which highlighted fears of relationship strain due to HIV-discordant results in couples25.
Conclusion
The study highlighted barriers and facilitators to HIV self-testing among Kenyatta University undergraduates, offering insights for interventions to boost self-testing uptake and enhance HIV prevention and care. Key barriers included fear of positive results, access challenges, and HIV stigma, while positive attitudes and media exposure were facilitators. Strategies should focus on reducing stigma, increasing self-test kit accessibility and affordability, improving counseling services, and addressing gender disparities in testing. HIV self-testing is advised as a supplementary approach to facility-based testing, with a need to monitor its long-term effects on prevention and treatment.
References
- 1.Ndabarora E, Mchunu G. (2014) Factors that influence utilisation of HIV/AIDS prevention methods among university students residing at a selected university campus.Sahara J. 11(1), 202-210.
- 3.NASCOP. (2019) An operational manual for the delivery of HIV Self-Testing services in Kenya.Who. Published online 40.
- 6.A. (2020) . Sund RB.National AIDS and STI Control Programme (NASCOP), Preliminary KENPHIA 2018 Report , Nairobi: NASCOP; 430-439.
- 7.JKW Wilbert, WANG Y P, HE M Y. (2016) Determinants of Students’ Uptake of Reproductive Health Services Targeting High Risk Sexual Behaviour in Kenyatta University,Nairobi County,Kenya.Journal of Knowledge Management. 2(2), 1-18.
- 8.Lee V J, Tan S C, Earnest A, Seong P S, Tan H H et al. (2007) User Acceptability and Feasibility of Self-Testing With HIV Rapid Tests.JAIDS Journal of Acquired Immune Deficiency Syndromes. 45(4), 449-453.
- 9.Chanda M M, Ortblad K F, Mwale M. (2017) HIV self-testing among female sex workers in Zambia: A cluster randomized controlled trial.PLoSMedicine. 14(11), 1-19.
- 10.Hatzold K, Gudukeya S, Mutseta M N. (2019) HIV self‐testing: breaking the barriers to uptake of testing among men and adolescents. in sub‐Saharan Africa, experiences from STAR demonstration projects in Malawi, Zambia and Zimbabwe.J Intern AIDS Soc. 22(S1): e25244 10-1002.
- 11.Buldeo P, Gilbert L. (2015) Exploring the Health Belief Model and first-year students’ responses to HIV/AIDS and VCT at a South African university.African. , Journal of AIDS Research 14(3), 209-218.
- 12.Denford S, Abraham C, Campbell R, Busse H. (2017) A comprehensive review of reviews of school-based interventions to improve sexual-health.Health Psychology Review. 11(1), 33-52.
- 13.Bassett Wilson D, Taaffe J, Freedberg K A. (2015) Financial incentives to improve progression through the HIV treatment cascade:Current Opinion. in HIV and AIDS 10(6), 451-463.
- 14.Elshiekh H F, H De Vries, Hoving C. (2021) Assessing sexual practices and beliefs among university students in Khartoum, Sudan; a qualitative study.SAHARA-J:. , Journal of Social Aspects of HIV/AIDS 18(1), 170-182.
- 15.Folasayo A, Oluwasegun A, Samsudin S, Saudi S, Osman M et al. (2017) Assessing the Knowledge Level, Attitudes, Risky Behaviors and Preventive Practices on Sexually Transmitted Diseases among University Students as Future Healthcare Providers in the Central Zone of Malaysia: A Cross-Sectional Study.IJERPH. 14(2), 159-10.
- 16.Marks S J, Merchant R C, Clark M A. (2021) Barriers to HIV Testing and Opportunities for Expansion Using Home-Based HIV Self-Testing: Results of a National Study of Higher HIV Risk Young Men Who Have Sex With Men.SAGE Open. 11(2), 215824402110168-10.
- 17.Qin Y, Han L, Babbitt A. (2018) Experiences using and organizing HIV self-testing.AIDS. 32(3), 371-381.
- 18.Clifton S, Nardone A, Field N. (2016) HIV testing, risk perception, and behaviour in the British population.AIDS. 30(6), 943-952.
- 19.Birdthistle I, Mulwa S, Sarrassat S. (2022) Effects of a multimedia campaign on HIV self-testing and PrEP outcomes among young people in South Africa: a mixed-methods impact evaluation of ‘MTV Shuga Down South.’BMJ Glob Health. 7(4), 10-1136.
- 20.Iwelunmor J, Ezechi O, Obiezu-Umeh C. (2020) The 4 youth by youth HIV self-testing crowd sourcing contest: A qualitative evaluation. Matovu JKB, ed.PLoSONE 15(5), 10-1371.
- 21.Mathews A, Farley S, Conserve D F. (2020) Meet people where they are”: a qualitative study of community barriers and facilitators to HIV testing and HIV self-testing among African Americans in urban and rural areas in North Carolina.BMC Public Health. 20(1), 494-10.
- 22.Indravudh P P, Choko A T, Corbett E L. (2018) Scaling up HIV self-testing in sub-Saharan Africa: a review of technology, policy and evidence.Current Opinion in Infectious Diseases. 31(1), 14-24.
- 23.Inwani I, Chhun N, Agot K. (2021) . Preferred HIV Testing Modalities Among Adolescent Girls and Young Women in Kenya.Journal of Adolescent Health 68(3), 497-507.
