Postpartum Ovarian Vein Thrombosis After Coronavirus Disease
Abstract
COVID-19 epidemic, described as a community health emergency by the World Health Organization, began in December 2019. COVID-19 is a source of deep vein thrombosis (DVT) because of hypercoagulation, blood stasis, and endothelium injury complications. This study reports a 26-year-old pregnant woman with coronavirus hospitalized with a left ovarian vein (LOV) thrombosis at Sultangazi- Haseki Training and Research Hospital in Istanbul. Risk classification for DVT disease is of crucial importance for the forecast of coronavirus.
Author Contributions
Academic Editor: Raul Isea, Fundación Instituto de Estudios Avanzados - IDEA, Hoyo de la Puerta, Baruta.
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2022 Murat Ekmez, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
In December 2019, the first case of COVID-19 pneumonia was reported in Wuhan, China’s Hubei Province, and the disease quickly spread to other parts of the world 1, 2. The new coronavirus SARS-CoV-2 is the source of the novel coronavirus infection COVID-19. An excessive inflammatory response is the characteristic feature of the virus. It can lead to severe manifestations such as adult respiratory distress syndrome, septicemia, coagulopathy, and death in some patients 3. Ovarian vein thrombosis (OVT) is a rare thrombotic condition that primarily affects postpartum women; It is usually manifested by fever and lower abdominal pain that occurs weeks after birth 4, 5.
Patients with COVID-19 are in the high-risk group of thrombosis due to their hypercoagulation, blood stasis, and endothelium injury 6. OVT is a severe and uncommon disease that can occur anywhen. It is more common in the period after childbirth than in other cases, and its frequency is about 1 in 2000–3000 labors 5. More than 80% of the after-childbirth thrombosis cases are in the right gonadal vein 7. Clinical symptoms such as abdominal pain, pyrexia, nausea, vomiting, and malaise are some of the symptoms of this type of thrombosis.
OVT is a condition that occurs in 0.02%–0.18% of pregnancies, and 80%–90% of it can be identified on the right side of the affected cases 4, 5, 6. Characteristic visualization findings on ultrasonography involve tubular, hypoechoic adnexal, and/or iliac fossa masses. MRI allowed imaging of the overall track of the ovarian veins in patients with an inconsequential CT scan or ultrasonography, offering improved sensitiveness and specificity (92% to 100% and 100%, respectively 7.
In that case, we delivered a live baby at the 39th week of a pregnant woman who had a Covid-19 infection at her 30th week of pregnancy. In light of the current literature, we treated the patient diagnosed with ovarian vein thrombosis after presenting with abdominal pain on the 10th postoperative day.
Case Presentation
A 25-year-old woman with a BMI index of 21 and a G4P3A1 (2 NSD, 1 C / S) delivered a cesarean section 10 days ago came to the hospital with the complaint of abdominal pain. In the patient’s history, it was learned that he was infected with COVID-19 when she was 30th gestational weeks and did not receive any antiviral treatment other than 4000 IU fraxiparine daily. There was not any history of illness or thrombosis in the patient’s medical history. The patient gave birth to a single live baby by cesarean in the 39th gestational week. She was discharged on the third-day post-op. After the onset of abdominal pain, one week later, she was transferred to our clinic.
During her hospitalization, the patient’s physical examination revealed sensitivity in the abdominopelvic check, a body warmth of 37.4 °C, blood pressure rate of 100/60 mm Hg, the pulse of 88 beats per minute, the respiratory rate of 14 breaths per minute, and blood oxygen saturation level of 95 percent at 5 liters per minute. Most routine blood tests, kidney function tests, electrolyte, and serum procalcitonin levels were regular. The COVID-19 PCR test performed during the delivery and hospitalization of the patient was negative. In routine blood tests, CRP values were 260, and WBC values were 11.61, as high.
In the transabdominal USG, the diameter of the LOV was enlarged, and thrombosis was observed with diffusion restriction in the lumen. In bilateral lower extremity Doppler USG, no appearance compatible with thrombus in the lower extremities was observed.
The abdomen and pelvis area were examined by MRI with contrast. It revealed a markedly dilated LOV containing abnormal soft tissue attenuation material throughout, indicating ovarian vein thrombosis. The aspect of a LOV in MRI images was persistent, with signs of increased signal in this area (Figure 1). Subsequent inferior abdominal MRI demonstrated a thrombus starting from the LOV to the level of the left renal vein. There is an enhancement in the vein walls (thrombophlebitis).
Figure 1.The appearance of a left ovarian vein in MRI.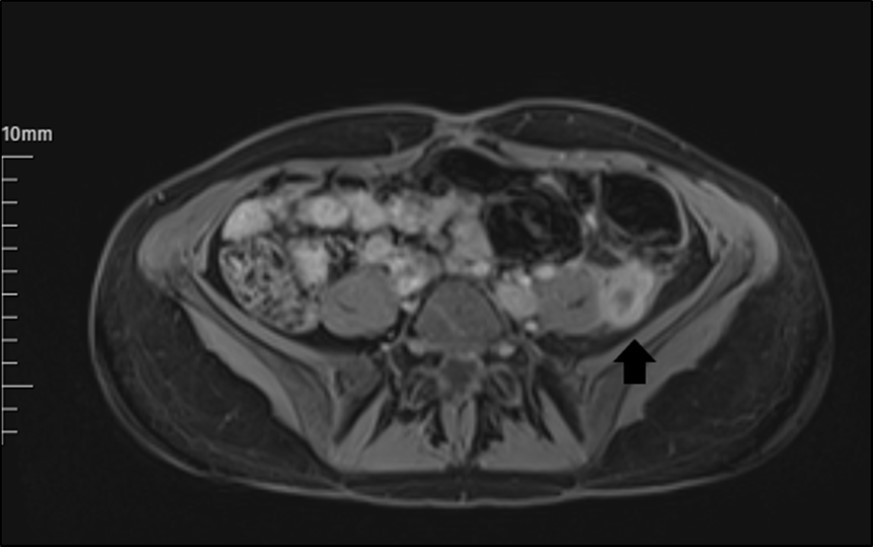
The patient took on 2X6000 fraxiparine as treatment. In addition, Genta, Klindan, and cefazoline were given to treat thrombophlebitis. One week after her hospitalization, the patient was discharged because the OVT decreased in MRI. The patient has been told that Fraxiparine should be remained on for one month as prophylactic. Upon, she was followed by the cardiovascular surgery clinic. In the lower abdomen MRI performed one month later, OVT was observed to have decreased significantly.
Discussion
OVT ensues in about 1 in 600 to 1 in 2000 pregnancies. It shows signs of as a triad of pain, fever, and abdominal mass 2. It is hypothecated that OVT generally occurs on the right side because the right ovarian vein (ROV) is longer than the LOV, and it lacks competency of the valves 2. The ROV enters the inferior vena cava at an acute angle, making it more susceptible to compression 4.
In our case, we found LOV thrombosis contrary to what is usually detected. This situation could be an indication of the low incidence of our case.
In terms of pathophysiology, many cases have demonstrated that patients with COVID-19 are generally vulnerable to lack of water to venous thrombosis due to pyrexia and diarrhea, hypotension, secondary infections, and extended rest cure. So, to decrease the complications and fatality rate from COVID-19, it is essential to value the risk of DVT.
It is worthy of mention that it is not seen any evidence of venous thrombosis in previous deliveries when the patient’s medical history was examined before COVID-19, and there were no recordings of the disease in the patient’s family. Therefore, it is considered that acute thrombosis like this occurred during the COVID-19 infection.
Our report attaches further documents on side reactions such as blockade of veins and arteries in a patient with COVID-19. Assessment and risk classification for DVT disease are critical for the prognosis of coronavirus disease.
The preliminary coagulopathy of COVID-19 shows a featured ascent of D-dimer and fibrin and fibrinogen-degradation products, whereas abnormalities in PT, PTT, and platelet counts are comparatively uncommon at first view. Clotting test screening, including evaluating D-dimer and fibrinogen levels, is recommended 8.
The most characteristic indication in patients with COVID-19 and coagulopathy is an heighten D-dimer concentration, a relatively moderate decrease in platelet count, and a extension of the PT 10.
Many patients with exquisite COVID-19 present with coagulation abnormalities that trigger other systemic coagulopathies associated with serious infections, such disseminated intravascular coagulation or thrombotic microangiopathies, but coronavirus has evident features 9.
Besides, OVT mainly occurs in the puerperium period due to postpartum endometritis and concomitant flow changes in the venous system (Hodgkinson CP, 1953).
Complications of symptomatic OVT comprise sepsis and thrombus extension (25% to 30%) to the inferior vena cava or left renal vein or rarely pulmonary embolism.
Asymptomatic OVT is more common and may be benign, with a 30% incidence of pelvic (iliac and ovarian) vein thrombosis stated on screening MRI after vaginal delivery 5. pyrexia was not accompanied in our case; blood culture was not studied.
The fact that the patient did not take any antiviral treatment when she had a COVID-19 infection at 30 weeks old, may have caused to the OVT that happened in the postoperative period. Perhaps, for this reason, the tendency to coagulation during pregnancy may have caused this rare condition to occur.
The patient was not in danger of having a DVT, and she had no history of vein thrombosis in both previous pregnancies and the postpartum period. Contrary to expectations, vein thrombosis in the LOV is observed instead of the ROV in the patient. Considering this situation, having a COVID-19 infection during pregnancy should be regarded as a risk factor for deep vein thrombosis.
Conclusion
COVID-19 is a source of DVT because of hypercoagulation, blood stasis, and endothelium injury complications. Risk stratification for DVT disease is vital for the preplan of coronavirus. The disease can be diagnosed with a Doppler ultrasound thoroughly. Nevertheless, if the diagnose is unclear, it can be entirely validated by CT and MRI. The primary basis of treatment is the conservative tendency, whereas the surgical movement is conceived for insisting on DVT. DVT is important to take into consideration in postpartum developing pelvic pain who had COVID-19 disease during pregnancy.
Compliance with Ethical Standards
The authors declare that there is no conflict of interest that prejudices the impartiality of this scientific work. No commercial or financial support has been received.
Abbreviations
Deep Vein Thrombosis: DVT
Right Ovarian Vein: ROV
Left Ovarian Vein: LOV
References
- 1.Zhu N, Zhang D, Wang W. (2019) A Novel Coronavirus from Patients with Pneumonia in. , China, N Engl J Med 382(8), 727-733.
- 2.Ahn D G, Shin H J, Kim M H, Lee S, Kim H S et al. (2020) . Current Status of Epidemiology, Diagnosis, Therapeutics, and Vaccines for Novel Coronavirus Disease 2019 (COVID-19). J Microbiol Biotechnol 30(3), 313-324.
- 3.Miesbach W, Makris M. (2020) COVID-19: Coagulopathy, Risk of Thrombosis, and the Rationale for Anticoagulation. Clin Appl Thromb Hemost. 26, 1076029620938149.
- 4.Tesfaye S, Tariku M, Hirigo A T. (2020) Postpartum left ovarian vein thrombosis. , SAGE Open Med Case Rep 8, 2050313-20962637.
- 5.BTS Bannow, Skeith L. (2017) Diagnosis and management of postpartum ovarian vein thrombosis. Hematology Am Soc Hematol Educ Program. 1, 168-171.
- 6.Rottenstreich A, Da’as N, Kleinstern G, Spectre G, Amsalem H et al. (2016) Pregnancy and non-pregnancy related ovarian vein thrombosis: Clinical course and outcome. Thromb Res. 146, 84-88.
- 7.Kubik-Huch R A, Hebisch G, Huch R, Hilfiker P, Debatin J F et al. (1999) Role of duplex color Doppler ultrasound, computed tomography, and MR angiography in the diagnosis of septic puerperal ovarian vein thrombosis. Abdom Imaging. 24(1), 85-91.
