Abstract
Objective:
Presentation of rare case report of primary non-Hodgkin Lymphoma of temporal bone secondary to immunodeficiency after prolonged steroid administration in a diabetic patient. Then review the literature of similar case reports.
Method:
49 years old female presented with hearing loss, facial paralysis and otalgia. Biopsy revealed high grade non Hodgkin’s B-lymphoma. She underwent chemotherapy and had remarkable response.
Result:
Rapidly progressive deafness, facial paralysis and otalgia are common presentations of external canal Non-Hodgkin lymphoma. The disease is common in middle age, females and has a fair response to chemotherapy, good to radiotherapy. Surgery is an alternative method in isolated lesions or recurrent cases.
Conclusion:
High dose steroid and type II diabetes are potential risks for acquired immunodeficiency. External Auditory canal lymphoma is uncommon sequel. Chemotherapy is very effective in treatment of isolated cases without B symptoms
Author Contributions
Academic Editor: Anil Tombak, Faculty of Medicine, Turkey. Email: [email protected]
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2018 Bassem A D, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Background
The head and neck is the second common sites of primary extranodal lymphoma after the abdomen. Sporadic cases originating from temporal bone have been reported. The potential sites in head and neck include middle ear, mastoid, internal auditory canal and external auditory canal.1
Case Presentation
A 49 years old Caucasian woman presented with a 3 week history of right ear deafness without tinnitus of acute onset and rapidly progressive course. The condition was associated with non nocturnal otalgia, rash in lower limbs (like livido reticularis) and right temporal headache. Then she developed right complete facial paralysis and bleeding from right ear. 2 week before the deafness, she had unexplained dizziness and collapse; for which she was admitted to the Acute Medical Unit . She had a carotid Doppler check on admission which was normal. No past history of trauma or any ear problems.
Her medical history include essential hypertension over last 2 years, type II diabetes mellitus for 3 years and refractory asthma that was treated with a heavy dose of oral prednisolone (25 mg daily) and inhaled steroid for 3 years. Accordingly she developed secondary adrenal insufficiency, iatrogenic Cushing syndrome, Osteopenia, osteoporosis and atrioventricular nodal reentrant tachycardia without cardiomegaly. She discontinued the steroid after her diagnosis of adrenal insufficiency that was few weeks prior to her ear problem. She also had a past history of ovarian neoplasm many years ago.
In the early stage of her deafness, her ear examination was surprisingly normal with intact tympanic membrane evan, the tympanogram was type “A” on both sides.
when the facial nerve paralysis started, it was House-Brackmann grade V/VI. The external canal was fully occluded with reddish-purple soft mass with bleeding on touch. (Figure 1). There was no redness or narrowing in external canal skin. No lymph nodes detected. Her nasal and throat examination was clear. The rest of neurological examination was normal. She didn’t have any weight loss nor night symptoms of increase temperature or sweat. The audiogram showed conductive hearing loss with air-bone gap 20 dB at 1000 Hz.
Figure 1.Right ear shows reddish-purple mass
Fractionated blood count showed mild anemia (Haemoglobin 103 g/L), slight leucocytosis 11.6x109/L, (N 4-11x109/L) with neutrophilia (Neuts 7.45×10 9/l, Lymphs 2.99×10 9/l, Mono 1.03×10 9/l, Eosins 0.14×10 9/l, Basos 0.03×10 9/l) and normal platelet count (390 x109/L).. Her liver (ALT 25 IU/L (N 5-65 iu/L), ALP 67/L (N 30 - 130 IU/L), Ptn 71 (N 60 - 80 g/L), billirubin 5 µmol/L), kidney functions (creatinine 56µmol/L (60–120 μmol/l), urea 5.4 mmol/L (N 2.5–6.6 mmol/l), eGFR >60 ml/min) were normal. The electrolytes (sodium 143 mmol/L, potassium 5.4 mmol/L) were normal as well. The C-reactive protein was slightly elevated (11.8 mg/l, N 0-5mg/L at 1 hour). Thiopurine Methyl Transferase (TPMT) was low (30 Um/L, N 68-150 um/L). HIV, EBV were tested with negative results.
Six Biopsies (3 mm) were taken from the mass of right ear under local anaesthesia. The histology was keratinised stratified squamous epithelium with underlying variable infiltrate of large atypical lymphoid cells suggestive of high grade non Hodgkin’s lymphoma (Figure 2).
Figure 2.Low/High Power H & E: Dermal infiltrate of large blastic lymphoid cells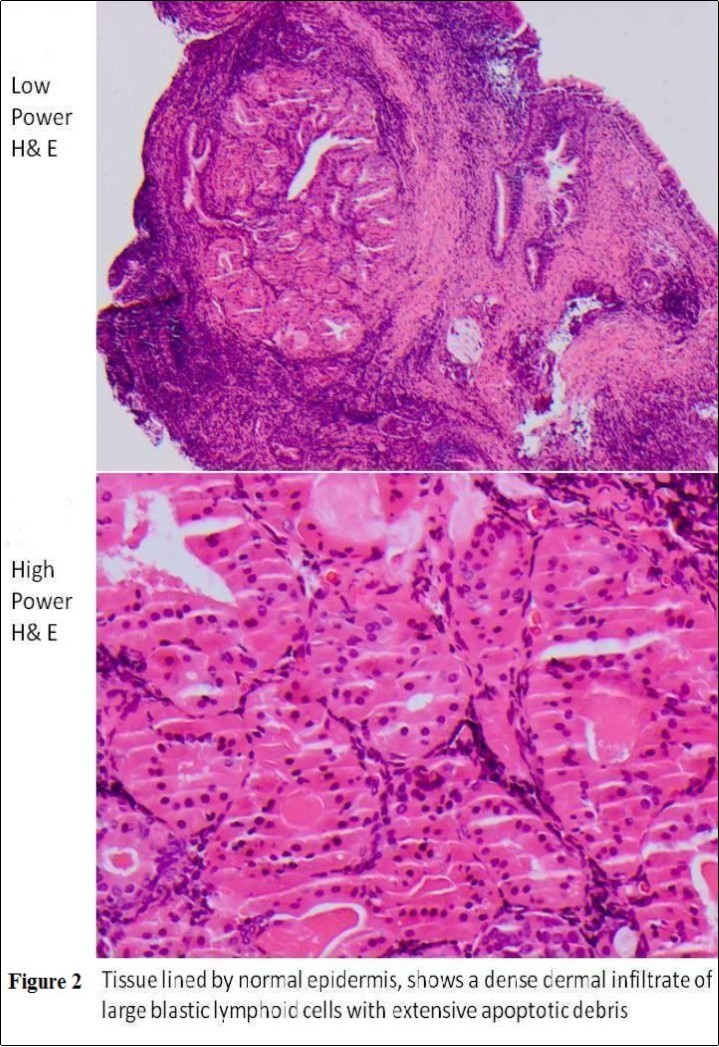
The immunohistochemical confirmed infiltrating lymphoid blasts CD45 positive, CD30 negative, cytokeratin negative and CD5 negative, CD20+ B lymphoid blasts with few scattered CD3+ T lymphocytes in the background. The B lymphocytes are CD79+a, CD5 weak +, CD10-, CD21-, CD23-, Bcl-2+, Bcl-6+, CD43-, MUM1+. Ki-67 staining shows a high proliferation index approaching 60%.
She had CT and MRI of her head. The CT showed occlusion of right external auditory canal with soft tissue mass with bone destruction superiorly. The soft tissue pushed the tympanic membrane into the middle ear which was itself pneumatised and free of the disease (Figure 3). The MRI detected intracranial extension into posterior fossa (Figure 4). She had also CT scan of neck, thorax, abdomen and pelvis for staging that didn’t show further disease.
Figure 3.Coronal CT head showing soft tissue occluding right EAC; bony destruction of the roof.
Figure 4.Axial MRI head showing extension from medial aspect of right EAC intracranially
Her final diagnosis was diffuse high grade large B-cell Non-Hodgkin lymphoma according to WHO classification with staging of IA (Ann Arbor Staging).
The patient received 3 doses of R-CHOP (Rituximab, cyclophosphamide, doxorubicin, vincristine, prednisolone) in regimen of once/3 weeks. She noticed improvement in otalgia, facial palsy and hearing after the first dose. After the second dose, hearing returned to normal and facial palsy recovered completely. No recurrence in 12 months follow-up.
Discussion
Non-Hodgkin lymphoma (NHL) in external Auditory canal is uncommon. Very few cases have been reported in relation to temporal bone. They can originate from internal auditory meatus, infratemporal fossa, middle ear, pinna and rarely from external auditory canal,2
Most of the non-Hodgkin lymphoma cases in temporal bone are associated with human Immunodeficiency virus (HIV) patients. Virtually, all cases of HIV-associated non-Hodgkin’s lymphoma are of B cell origin; approximately half of these cases are extranodal in presentation.3 The exact reason is unknown but may relate to perturbations of various adhesion molecules. LFA-1 (lymphocyte function-associated antigen 1) and LFA-3 (lymphocyte function-associated antigen 3) are down regulated specifically in the neoplastic cells. Elevated serum IL6 have been associated with the development of lymphoma as HIV stimulate the production IL6 production.4 The disease often has rapid progression and usually of high-grade.3
Prolonged high dose of steroid treatment can result in agranulocytosis with acquired immunodeficiency.1 It was implicated for the development of NHLin some case-control studies in late 1990’s and early 2000’s. A large series of case control study in Sweden in 2005 for patients who were taking prednisolone regularly up to 100 mg daily ruled out the increased risk of lymphoma for these patients. 5 Another latest study showed steroid and immunosuppressant could increase the risk of lymphoma for conditions such as inflammatory bowel disease and autoimmune disorders 6. Type II diabetes has 20% increase risk of blood cancer 7. In the current case report, the reason for the lymphoma was unclear; we speculate the link to co-morbidities of long term steroid and underlying diabetes; especially with the development of secondary acquired adrenal insufficiency and Cushing syndrome. There are limited case reports which showed that cushing syndrome can mask the progression of NHL. 8 The endocrine dysfunction should be considered a warning sign to every physician for remodelling steroid treatment.
The diagnosis of extranodal lymphoma of head & neck particularly the ear is difficult because the disease usually mimics other conditions such as squamous cell carcinoma or necrotizing otitis externa (NOE). In addition the diagnostic criteria for malignant lymphoid infiltrate is absent in the extranodal types. Thus the panel of markers in the immunohistochemistry (IHC) with various antibodies should be considered the investigation of choice with such presentation.1
The non-Hodgkin lymphoma of temporal bone usually presents with hearing loss and facial paralysis.1, 3 Vertigo and ear fullness are also reported in some cases as initial presentation.2 Otalgia can be the presenting symptom with/out deafness even before the development of facial paralysis. This is the common presentation for external ear canal in HIV-positive patients.1, 4 Localized swelling or lymph nodes are noted only in few cases.9
The current report has the typical presentation of early deafness and facial paralysis. The lymphoma has a rapid progressive course in the ear than any other skin malignancy. The presentation is different from any inflammatory condition. It lacks the typical deep nocturnal otalgia of NOE in addition to the resistance to medical treatment. The soft tissue mass of external canal is grossly different from the granulation in NOE or the polyp of middle ear cholesteatoma. It is deep purple large mass and bleeds easily on touch. Finally, skin of external canal won’t show signs of acute inflammation. It isn’t hard to say that superimposed infection will make clinical diagnosis difficult. It is always recommended to biopsy any persistent polyp after treatment or any mass in external auditory canal especially in immune compromised patients.
The prognosis of non-Hodgkin lymphoma of external ear varies a lot depending on the etiology, type of lymphoma, site of origin, staging and presence of B symptoms. In HIV-related patients, the poor prognostic indicators are the decreased CD4 lymphocytes, presence of acquired immunodeficiency syndrome prior to lymphoma development, extent of disease and the use of intensive chemotherapy which is found to worsen the already profound immunodeficiency. If left untreated, the average survival time is one month. Radiotherapy is appropriate for an isolated case that may extend survival to 1.5 year.4 Surgery is not recommended in this group.4, 10
In non-HIV related cases, survival time is shortened with increased tumor bulk, presence of systemic “B” symptoms and old age. In isolated lesions, radiotherapy showed better results than chemotherapy. With Radiotherapy, no recurrence was noticed after 9 years of treatment, 1 while recurrence was noticed after chemotherapy which managed later by surgical resection.2 Generally, B-cell lymphomas have a better prognosis than T-cell lymphomas, because chemotherapy is effective for the B-cell type. Surgical excision is an alternative option especially in non-HIV cases with contraindication to radiotherapy or failure of chemotherapy.3
Chemotherapy however showed promising results in middle ear lymphoma whether alone or combined with other modalities such as radiotherapy and surgery.9, 11
In this case, the patient didn’t have any “B” symptoms on presentation. After she completed 3 courses of R-CHOP, the lymphoma regressed totally from her ear. The full recovery of hearing and facial function after 2 doses illustrate good prognosis and the patients should be reassured about prognosis of their hearing and face movement. In addition, these two symptoms can be used as indicators for the response to the chemotherapy. She had now 12 months post treatment with disease free. However, continue monitoring for 5 years is still recommended.
38 case reports are present in the literature of primary temporal bone involvement. 12 are related to internal auditory canal, 17 involved middle ears and only 9 cases reported in external auditory canal (Table 1).
Table 1. Summary of primary lymphoma of temporal bone (external canal)| No | Age | Gender | Risk | Therapy | Outcome | Reference |
| 1 | 74 | F | No | CT, RT | Alive | 7 |
| 2 | 38 | M | HIV | CT | Died | 8 |
| 3 | 83 | F | No | RT | Alive | 1 |
| 4 | 49 | M | No | CT, S | Recur | 3 |
| 5 | 53 | F | No | S, CT | Recur | 2 |
| 6 | 36 | F | HIV | RT | Died | 4 |
| 7 | 46 | M | No | S, CT | Alive | 9 |
| 8 | 53 | F | No | S, CT | Alive | 10 |
| 9 | M | No | CT | Alive | 11 | |
| 10 | 49 | F | No | CT | Alive | Case Study |
From Table 1, NHL commonly affects females in middle age. There is no international guidelines on the mode of treatment however chemotherapy alone or combined with surgery is frequently used. Radiotherapy can also be used together with chemotherapy.
Conclusion
Steroid and diabetes are risk factors for acquired immunodeficiency that can result in extranodal NHL of the ear. Acute hearing loss and facial paralysis with a mass in external auditory canal are alarming features for non-Hodgkin lymphoma. Immunohistochemistry is the preferred marker for non-Hodgkin lymphoma. Chemotherapy is very effective in isolated cases without B-symptoms.
References
- 1.Hersh S P, Harrison W G, Hersh D J. (2006) Primary B cell lymphoma of the external auditory canal. , Ear Nose Throat J 85(9), 597-9.
- 2.Fish B M, Huda R, Dundas S A. (2002) B-cell lymphoma of the external auditory meatus. , J Laryngol Otol 116(1), 39-41.
- 3.Shuto J, Ueyama T, Suzuki M. (2002) Primary lymphoma of bilateral external auditory canals. , Am J Otolaryngol 23(1), 49-52.
- 4.Kieserman S P, Finn D G. (1995) Non-Hodgkin's lymphoma of the external auditory canal in an HIV-positive patient. , J Laryngol Otol 109(8), 751-4.
- 5.Askling J, al Et.Do steroids increase lymphoma risk? A case–control study of lymphoma risk in polymyalgia rheumatica/giant cell arteritis. Ann Rheum Dis.2005Dec;. 64(12), 1765-1768.
- 7.Castillo J J, Mull N, Reagan J L. (2012) Increased incidence of non-Hodgkin lymphoma, leukemia, and myeloma in patients with diabetes mellitus type 2: a meta-analysis of observational studies. , Blood 119(21), 4845-50.
- 8.al.Custing's syndrome can precipitate diabetes but mask non-Hodgkin's lymphoma. , Med J Aust.2008Feb18; 188(4), 262.
- 9.Ogawa S, Tawara I, Ueno S. (2006) De novo CD5-positive Diffuse Large B-cell Lymphoma of the Temporal Bone Presenting with an External Auditory Canal Tumor. , Intern Med. Epub2006Jul3 45(11), 733-7.
- 10.Goodarzi M O, Broberg T G, Lalwani A K. (1998) Lymphoma of the tympanic membrane in acquired immunodeficiency syndrome. Auris Nasus Larynx. 25(1), 89-94.
- 11.Bruschini Luca, Andrea De Vito, Fortunato Susanna. (2013) A Case of Primary Non-Hodgkin's Lymphoma of the External Auditory Canal. Case Rep Otolaryngol.2013:. 138397.
